Interstitial Lung Disease(ILD)
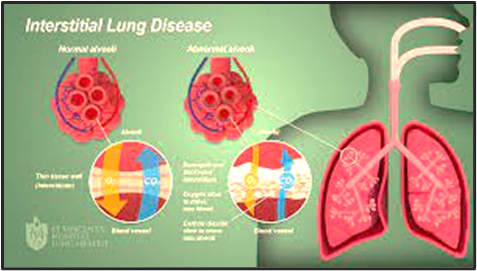
Interstitial Lung Disease(ILD) is a group of many lung conditions. All interstitial lung disease affect the interstitium, a part of your lungs.
The interstitium is a lace-like network of tissue that goes throughout both lungs It supports your lungs tiny air sacs, called alveoli. Normally, the interstitium is so thin that it doesn’t show up on X-rays or CT scans.
Interstitial
(in-tur-STISH-ul) lung disease describes a large group of disorders, most of
which cause progressive scarring of lung tissue. The scarring associated with
interstitial lung disease eventually affects your ability to breathe and get
enough oxygen into your bloodstream.
Interstitial lung disease (ILD), sometimes also called
as diffused parenchymal diseases, Diffuse
parenchymal lung disease; Alveolitis; Idiopathic pulmonary pneumonitis (IPP) describes a heterogeneous collection of
distinctive lung disorders classified on the grounds of shared clinical,
radiographic, physiologic or pathologic factors.
Types of ILD
The classification system used to describe
interstitial lung disease categorizes conditions based on clinical,
histopathological or radiologic parameters.
Ø Clinical classification groups ILD by its causes to
help differentiate exogenous or endogenous factors.
Ø Interstitial lung disease diseases without
identifiable causes get grouped under idiopathic/primary which uses the histopathological
and radiological approach as its infrastructure.
All forms of interstitial lung
disease cause the interstitium to thicken. This can happen from inflammation,
scarring, or a build-up of fluid. Some forms of ILD last a short time (acute); others
are long-term (chronic) and don’t go away.
Some types of interstitial
lung disease include:
v Interstitial Pneumonia Bacteria, viruses, or fungi can infect the interstitium.
A bacteria called Mycoplasma pneumoniae is the most
common cause.
v Idiopathic pulmonary fibrosis. This makes scar tissue grow
in the interstitium. Experts don’t know what causes it.
v Nonspecific interstitial
pneumonitis. This is an
interstitial lung disease that often affects people with autoimmune conditions
such as rheumatoid arthritis or scleroderma.
v Hypersensitivity pneumonitis. This happens when
dust, mold, or other things that you breathe irritate your lungs over a
long time.
v Cryptogenic organizing
pneumonia (COP). COP is a pneumonia-like
interstitial lung disease without an infection. You might hear your doctor call
this bronchiolitis obliterans with organizing pneumonia (BOOP).
v Acute interstitial
pneumonitis. This is a
sudden, severe interstitial lung disease. People who have it often need to be
connected to a machine called a ventilator that breathes for them.
v Desquamative interstitial
pneumonitis. This is an
interstitial lung disease that partly results from smoking.
v Sarcoidosis. This causes interstitial
lung disease along with swollen lymph nodes. It can also affect your heart, skin,
nerves, and eyes.
Asbestosis. This is an interstitial
lung disease caused by breathing asbestos, a fiber used in building
materials.
ILD Causes
The cause of most interstitial
lung disease is unknown.
Bacteria, viruses, and fungi
can cause interstitial pneumonia. You can also get ILD if you regularly breathe
in things that can bother your lungs. These include:
- Asbestos
- Bird proteins (such as
from exotic birds, chickens, or pigeons)
- Coal dust or various
other metal dusts from working in mining
- Grain dust from farming
- Silica dust
- Talc.
Many
drugs can damage your lungs, especially:
·
Chemotherapy
drugs. Drugs designed to kill
cancer cells, such as methotrexate (Otrexup, Trexall, others) and
cyclophosphamide, can also damage lung tissue.
·
Heart
medications. Some drugs used to treat
irregular heartbeats, such as amiodarone (Nexterone, Pacerone) or propranolol
(Inderal, Innopran), may harm lung tissue.
·
Some
antibiotics. Nitrofurantoin (Macrobid,
Macrodantin, others) and ethambutol (Myambutol) can cause lung damage.
·
Anti-inflammatory
drugs. Certain anti-inflammatory
drugs, such as rituximab (Rituxan) or sulfasalazine (Azulfidine), can cause
lung damage.
Lung
damage can also result from autoimmune diseases such as:
·
Rheumatoid arthritis
·
Scleroderma
·
Dermatomyositis and polymyositis
·
Mixed connective tissue disease
·
Sjogren's syndrome
·
Sarcoidosis
It’s rare, but certain drugs
can cause ILD:
- Some antibiotics, like
nitrofurantoin
- Some anti-inflammatory
drugs, like rituximab
- Chemotherapy drugs like
bleomycin
- Heart medications such as
amiodarone
Anyone can get interstitial
lung disease, but some things can put you at higher risk:
- Age. Adults are much more likely to get
ILD, but children can, too.
- Autoimmune disease like lupus, rheumatoid
arthritis, and scleroderma
- Gastroesophageal reflux
disease (GERD)
- Genetics. Some conditions are passed down
among family members.
- Smoking
- Radiation treatments for cancer.
Symptoms
Ø
Shortness of breath is a main symptom of ILD. You may breathe
faster or need to take deep breaths:
Ø At first,
shortness of breath may not be severe and is only noticed with exercise,
climbing stairs, and other activities.
Ø Over time,
it can occur with less strenuous activity such as bathing or dressing, and as
the disease worsens, even with eating or talking.
Ø
Most people with this condition also have a dry cough. A dry
cough means you do not cough up any mucus or sputum.
Ø
Over time, weight loss, fatigue, and muscle and joint pain are
also present.
Ø
People with more advanced ILD may have:
Ø Abnormal
enlargement and curving of the base of the fingernails (clubbing).
Ø Blue colour
of the lips, skin, or fingernails due to low blood oxygen levels (cyanosis).
Ø Symptoms of
the other diseases such as arthritis or trouble swallowing (scleroderma),
associated with ILD.
Exams and Tests
The health care provider will perform a physical exam. Dry,
crackling breath sounds may be heard when listening to the chest with a
stethoscope.
The following tests may be done:
Ø Blood tests
to check for autoimmune diseases
Ø Bronchoscopy
with or without biopsy
Ø Chest x-ray
Ø High
resolution CT (HRCT) scan of the chest
Ø MRI chest
Ø Echocardiogram
Ø Open lung
biopsy
Ø Measurement
of the blood oxygen level at rest or when active
Ø Blood gases
Ø Pulmonary
function tests
Ø Six-minute
walk test (checks how far you can walk in 6 minutes and how many times you need
to stop to catch your breath)
People who are heavily exposed to
known causes of lung disease in the workplace are usually routinely screened
for lung disease. These jobs include coal mining, sand blasting, and working on
a ship.
MANAGEMENT
AND TREATMENT
There’s no cure for interstitial lung disease. Treatment for ILD
usually focuses on treating underlying disease and improving your symptoms.
Your healthcare provider might prescribe physical therapy, supplemental oxygen
or medication to reduce inflammation or slow down the disease.
Medications.
- Corticosteroids. Drugs like
prednisone can help reduce inflammation.
- Anti-fibrotic and
cytotoxic drugs. These medications can slow down lung scarring. They
include azathioprine, cyclophosphamide, pirfenidone and nintedanib.
- Biologic drugs. Medications like
rituximab are sometimes used to treat autoimmune diseases and other
causes of ILD.
- Treatment for GERD. Gastroesophageal
reflux disease (GERD) can make ILD worse, so your provider may
prescribe medications to keep stomach acid down.
- Pulmonary rehabilitation. Breathing exercises
and physical therapy can make your lungs stronger and breathing easier.
- Oxygen therapy. Your provider
will prescribe extra oxygen if you don’t have enough getting to your blood
or tissues. It’s delivered through a mask or tube in your nose.
Some treatments for interstitial lung disease can weaken your
immune system. Your doctor will monitor you closely for complications if you’re
taking one of these medications.
Treatments for Interstitial Lung Disease
The treatment you get depends
on the type of ILD you have and its cause.
Antibiotics. These treat most
interstitial pneumonias. Pneumonias caused by a virus usually get better
on their own. Pneumonias caused by a fungus are rare but are treated with
antifungal drugs.
Corticosteroids. In some forms of
interstitial lung disease, inflammation in your lungs causes damage
and scarring. Corticosteroids cause your immune system’s activity to slow.
This lessens the amount of inflammation in your lungs and the rest of your
body.
Inhaled oxygen. If you have low oxygen
levels because of interstitial lung disease, inhaled oxygen may help your
symptoms. Regular use of oxygen might also protect your heart from damage
caused by low oxygen levels.
Lung transplant. In advanced interstitial
lung disease that has severely impaired you, you may need a lung transplant.
Most people who have a lung transplant for interstitial lung disease make large
gains in their quality of life and their ability to exercise.
Azathioprine (Imuran). This drug also slows
down the immune system. It’s not shown to improve interstitial lung disease,
but some studies suggest it might help.
N-acetylcysteine (Mucomyst). This potent antioxidant
may slow the decline of lung function in some forms of interstitial lung
disease. You’ll take it in combination with other treatments.
Other drugs are considered controversial
for interstitial lung disease treatment, including:
- Cyclophosphamide (Cytoxan)
- Cyclosporine
- Methotrexate
- Nintedanib (Ofev)
- Pirfenidone (Esbriet)
These medicines affect
the way your immune system works. If your doctor thinks you need one, they’ll
keep a close watch on you while you’re taking it. These medications can have
serious side effects.
Complications
Interstitial lung disease can
lead to a series of life-threatening complications, including:
·
High
blood pressure in your lungs (pulmonary hypertension). Unlike systemic high blood pressure, this condition
affects only the arteries in your lungs. It begins when scar tissue or low
oxygen levels restrict the smallest blood vessels, limiting blood flow in your
lungs. This in turn raises pressure within the pulmonary arteries. Pulmonary
hypertension is a serious illness that becomes progressively worse.
·
Right-sided
heart failure (cor pulmonale). This
serious condition occurs when your heart's lower right chamber (right
ventricle) — which is less muscular than the left — has to pump harder than
usual to move blood through obstructed pulmonary arteries. Eventually the right
ventricle fails from the extra strain. This is often a consequence of pulmonary
hypertension.
·
Respiratory
failure. In the end stage of chronic
interstitial lung disease, respiratory failure occurs when severely low blood
oxygen levels along with rising pressures in the pulmonary arteries and the
right ventricle cause heart failure.
PREVENTION
Many
causes of interstitial lung disease aren’t preventable. You can reduce your
risk of ILD by managing underlying conditions and avoiding breathing in harmful
substances.
- Avoid
or wear a respirator (a mask that filters particles from the air) when
working around harmful substances, such as asbestos, metal dusts or
chemicals.
- Avoid
or wear a respirator when working around things that can cause chronic
allergic reactions, like hay, grain, bird droppings or feathers and
heating and cooling systems.
- If
you have a connective tissue disease or sarcoidosis, talk to your
healthcare provider about ways to manage your illness to prevent ILD.
- Don’t
smoke or quit smoking.
Life expectancy
The life expectancy for interstitial lung
disease depends on the cause and severity. Some people with mild ILD can live
normal lives without treatment or with minimal treatment. Your outlook
(prognosis) is better if your disease isn’t getting worse (it’s stable).
For people with the most severe and rapidly
worsening forms of interstitial lung disease, life expectancy is around 3-5
years after diagnosis.







Comments
Post a Comment